56 yo man with 3 month history of a friable tumor mid lower lip. Non smoker. Works frequently outdoors for years. He has a history of BCC on his back.
O/E: 1 cm nodule lower lip. No palpable regional adenopathy
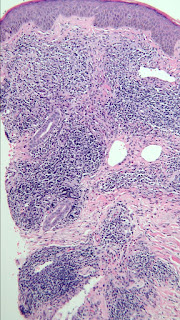
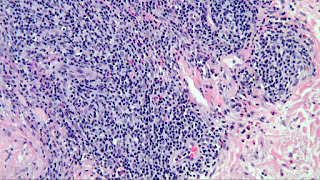
Pathology: Biopsy shows a moderately differentiated SCC with invasion into muscle but no definite perineural invasion or lymphatic invasion on the biopsy. [3 mm punch biopsy may not be representative of the true picture.]
Diagnosis: SCC lower lip, moderately differentiated.
Plan: Refer for micrographic surgery.
Questions:
1. Lip SCC < 2 cm diameter are reported to be at little risk for metastasis. With cases like this should an oncologist be consulted?
2. Is there a role for imaging preoperative imaging?
3. What cosmetic effects of surgery should the patient expect?
References::
1. Squamous Cell Carcinoma of the Lip-A Review of Squamous Cell
Carcinogenesis of the Mucosal and Cutaneous Junction. James P Bota. Dermatol
Surg. 2017 Apr;43(4):494-506. PMID: 28157733
Abstract: Background: The lip is an anatomic junction for 2
disparate groups of cancer. Cutaneous squamous cell carcinoma (cSCC) is a
common malignancy with a favorable prognosis, whereas oral-mucosal squamous
cell carcinoma (omSCC) is associated with significantly higher rates of nodal
disease and worse outcomes. The squamous cell carcinoma of the lip (lip SCC) is
more aggressive than cSCC but less aggressive than omSCC. However, work-up and
treatment vary between specialties.
Conclusion: Lip
SCC is an overlapping entity that poses many challenges to clinicians.
Specialists should be aware of current staging modalities as well as imaging
and treatment recommendations to optimize patient outcomes.
Comments from two respected
Moh’s surgeons:
1. In part it
depends on the depth of invasion. But without perineural invasion, PNI,
(defined as SCC cells within the perineural sheath, nerve diameter >0.1 mm
if intradermal or involving a sub-cutaneous nerve), this is a low risk lesion.
With no palpable adenopathy, imaging is not indicated. Neither is an
Oncologist. Mohs surgery or an excision with complete peripheral margin exam is
the recommended treatment. If Mohs is done, the remaining clinically
obvious tumor can be debulked and sent to path for further review for PNI.
Cosmetic insult should be low. If not invading muscle, mucosal advancement
flaps can usually close it elegantly. If muscle involved we often do a full
thickness "v" wedge repair of the lip. You can close a defect
involving 40% of the lip without microstomia and this lesion won't remove even
20%. The lip stretches back to its normal size in a few months. I'm on the NCCN
nonmelanoma skin cancer Guidelines of Care committee. We just finished our annual
review of the guidelines, which of course cover cSCC an hour ago! So you are
getting the most up to date info that can possibly be obtained!
2.
This patient looks to have a pretty straightforward case of a SCC on the
lip. I don't think you need to refer to
oncology or do imaging, given size of tumor,
no palpable nodes, no aggressive histology. He needs Mohs and needs it ASAP, as this has
grown to 1 cm size in 3 months. Give the Mohs surgeon a heads up that this is
growing relatively rapidly. The patient
wouldn't want it to increase significantly in size while he's waiting for an
appt. This is someone I would have
normally given priority to, given the chance for rapid growth. The lower lip is pretty forgiving and if this
SCC doesn't grow significantly, the defect could likely be brought together
primarily. One can remove up to a third
of the lower lip and close primarily without causing microstomia. We know the tumor is into muscle (common on
the lip, given thin overlying skin and minimal sc fat), but removing a wedge of
muscle will actually help minimize tension on the closure. Tell him stitching will extend into mouth and
below the vermillion (to correct the standing cones created with closure). I will send in a separate email a few photos
of some prior patients I have closed primarily with this type of defect. Took photo of a scrapbook page, so it may be
a little distorted.
I
would follow this fellow for the first year after surgery fairly closely (say,
q 3 mo) and feel for any palpable nodes.