We have been having technical problems with VGRD and have elected to publish this case here. Your comments will be appreciated -- please mail them directly DJ Elpern and we will post them to VGRD when it is up and running,
78 yo man with episodic incapacitating pruritus
Duration: 4 years
Distribution: Generalized, but sparing head and feet
The patient is a 78-year-old semi-retired music producer who presents with a four-year history of episodic intense pruritus that is generalized but has spared the face and the feet. It may have begun on the brachioradial areas of the arms but over a period of time spread to involve the sacrum, the chest, the back and the legs. He describes “a burning itch that you just cannot ignore.” At times he has “gone into a panic” over this. The itch can feel like “hot needles” applied to certain areas of the skin. He has also had scrotal pruritus for two years
The patient has seen a number of different physicians for this including four dermatologists. He has had biopsies done with nonspecific findings and direct and indirect immunofluorescence studies also have been noncontributory. There have been positive ANAs but no one has been able to correlate those with his pruritus.
His brother, has a similar problem and has been treated with CsA and azathioprine with good results.
Treatment:
1. multiple antihistamines -†no help.
2. multiple topical steroids -†no help.
3. Gabapentin - caused severe dizziness...unable to use.)
4. prednisone, three courses - resolved or alleviated symptoms.
(though less completely the second and third time.)
5. plaquenil, one month†- no help.
6. naltrexone, 2 weeks†- no help.
7. dapsone, 2 weeks†- no help.
8. pentoxifylline 400 qd x 2 weeks†- no help.
9. cellcept 2000 mg x 19 days†- no help.
10. Local heat hot compress seems to resolve it quickly though only temporarily).
11. Immuran
O/E: Excoriated papules – some crusted. Arms, legs, lower back, sacrum – sparing mid back, face. No vesicles or bullae.
Bx:
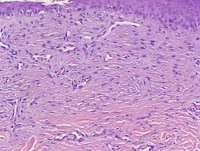
A superficial perivascular and interstitial lymphocytic infiltrate with scattered eosinophils and occasional neutrophils . Note : These changes are urticarial in nature. The histologic differential diagnosis includes urticaria or a dermal hypersensitivity reaction such as a drug eruption or insect bite reaction. Clinico-pathologic correlation is suggested.
Duration: 4 years
Distribution: Generalized, but sparing head and feet
The patient is a 78-year-old semi-retired music producer who presents with a four-year history of episodic intense pruritus that is generalized but has spared the face and the feet. It may have begun on the brachioradial areas of the arms but over a period of time spread to involve the sacrum, the chest, the back and the legs. He describes “a burning itch that you just cannot ignore.” At times he has “gone into a panic” over this. The itch can feel like “hot needles” applied to certain areas of the skin. He has also had scrotal pruritus for two years
The patient has seen a number of different physicians for this including four dermatologists. He has had biopsies done with nonspecific findings and direct and indirect immunofluorescence studies also have been noncontributory. There have been positive ANAs but no one has been able to correlate those with his pruritus.
His brother, has a similar problem and has been treated with CsA and azathioprine with good results.
Treatment:
1. multiple antihistamines -†no help.
2. multiple topical steroids -†no help.
3. Gabapentin - caused severe dizziness...unable to use.)
4. prednisone, three courses - resolved or alleviated symptoms.
(though less completely the second and third time.)
5. plaquenil, one month†- no help.
6. naltrexone, 2 weeks†- no help.
7. dapsone, 2 weeks†- no help.
8. pentoxifylline 400 qd x 2 weeks†- no help.
9. cellcept 2000 mg x 19 days†- no help.
10. Local heat hot compress seems to resolve it quickly though only temporarily).
11. Immuran
O/E: Excoriated papules – some crusted. Arms, legs, lower back, sacrum – sparing mid back, face. No vesicles or bullae.
Bx:
A superficial perivascular and interstitial lymphocytic infiltrate with scattered eosinophils and occasional neutrophils . Note : These changes are urticarial in nature. The histologic differential diagnosis includes urticaria or a dermal hypersensitivity reaction such as a drug eruption or insect bite reaction. Clinico-pathologic correlation is suggested.
Diagnosis: Uncertain. Possibly Subacute Prurigo
Reason Presented:
For diagnostic and therapeutic suggestions.. Have you seen similar cases? What has been the outcome?
DISCUSSION: All of his dermnatologists thought of D.H. but the biopsies have not confirmed this and dapsone and gluten free diet have not helped.
Please respond directly to DJ Elpern
Reason Presented:
For diagnostic and therapeutic suggestions.. Have you seen similar cases? What has been the outcome?
DISCUSSION: All of his dermnatologists thought of D.H. but the biopsies have not confirmed this and dapsone and gluten free diet have not helped.
Please respond directly to DJ Elpern