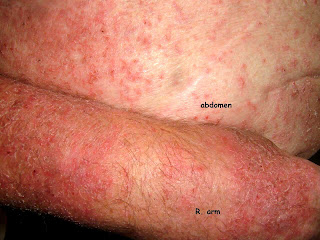
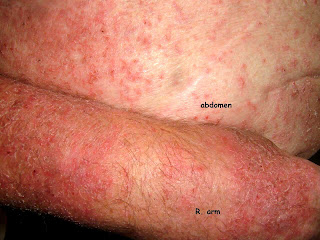
This 83 yo old man has chronic renal failure with a creatinine of 18 (!!) but does not need dialysis yet. His hemoglobin has been maintained with Procrit for the past four years. Because of a low transferrin saturation (30 %), his nephrologist added a new form of iron infusion around 2 months ago. (This was in another state and I don't have the name of the product) Within two weeks he started developing a generalized pruritic eruption. He stopped the iron infusions, but the rash persists.
There is only one report of a similar process (see below); but it is likely that more cases are extant as this therapy becomes more popular.
For the time being, he will be treated with triamcinalone 0.1% ointment after soaking in a tub. This is William James et. al's "Soak and Smear" technique. (see ref)
It's likely that the iron will stay in his system for some time. There are no treatment guidelines here; and as the patient can sleep at night, I prefer not to give him antihistamines at this time.

 Reference
Reference1.
The safety and efficacy of ferumoxytol therapy in anemic chronic kidney disease patients.Spinowitz BS, Schwenk MH,Jacobs PM et al
Kidney Int. 2005 Oct;68(4):1801-7.
BACKGROUND: Administration of safe and effective iron therapy in patients with chronic kidney disease is a time consuming process. This phase II clinical trial studied ferumoxytol, a semi-synthetic carbohydrate-coated iron oxide administered by rapid intravenous injection to anemic chronic kidney disease patients (predialysis or undergoing peritoneal dialysis). METHODS: Inclusion criteria included hemoglobin < or =12.5 g/dL and transferrin saturation < or =35%. Twenty-one adult patients were randomized to receive ferumoxytol in a regimen of 4 doses of 255 mg iron in 2 weeks or 2 doses of 510 mg iron in 1 to 2 weeks. Ferumoxytol was administered at a rate of up to 30 mg iron/sec. RESULTS: The maximum hemoglobin response following ferumoxytol administration occurred at 6 weeks, increasing from a baseline of 10.4 +/- 1.3 g/dL to 11.4 +/- 1.2 g/dL (P < 0.05). Ferritin increased from a baseline of 232 +/- 216 ng/mL to a maximum of 931 +/- 361 ng/mL at 2 weeks (P < 0.05), while the baseline transferrin saturation increased from 21 +/- 10% to 37 +/- 22% at 1 week (P < 0.05). Seven adverse events in 5 patients during this trial were deemed possibly related to ferumoxytol, none serious. These events included constipation, chills, tingling, a gastrointestinal viral syndrome,
delayed pruritic erythematous rash, and transient pain at the injection site. CONCLUSION: Although larger studies are required, this small study demonstrates that ferumoxytol can be safe and effective in increasing iron stores, is associated with an increased hemoglobin response, and is well tolerated at a rapid infusion rate.
2.
Soak and smear: a standard technique revisited. Gutman AB, Kligman AM, Sciacca J, Arch Dermatol. 2005 Dec;141(12):1556-9
BACKGROUND: Atopic dermatitis, nummular eczema, chronic hand dermatitis, palmar plantar psoriasis, and xerotic eczema are common inflammatory skin conditions. They may be refractory to conventional topical and even systemic treatment. Little evidence is available that demonstrates the benefits of aggressive topical treatment of patients with these disorders. OBJECTIVE: To describe a simple, inexpensive, effective topical treatment with an accompanying patient educational sheet. DESIGN: A retrospective study of 28 patients referred to a tertiary care center for refractory chronic pruritic eruptions. Intervention with a plain water 20-minute soak followed by smearing of mid-strength to high-strength corticosteroid ointment led to clearing or dramatic improvement. RESULTS: Objective and symptomatic improvement was obtained from aggressive topical treatment. It was well accepted in this group of referral patients. CONCLUSIONS: Hydration for 20 minutes before bedtime followed by ointment application to wet skin and alteration of cleansing habits is an effective method for caring for several common skin conditions. Prospective studies are needed to further validate these findings.