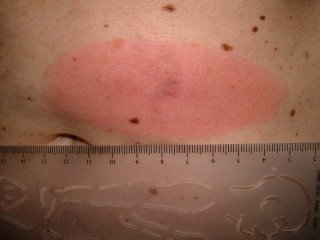
The patient is an 85 yo man who presented for generalized pruritus which has been present for two years. He has a history of prostate cancer and gastrointestinal bleeding. He's had a few transfusions over the past year or so and was concerned that they caused his itching.
He did not complain about his nose. I asked about it and he and his daughter gave this history: Three years ago he was hospitalized for pneumonia. He delvelped an inflammation of the ala nasi and was told it was "shingles." Biopsies were done and ruled out cancer. The left ala nasi was destroyed and this is how he healed.
Discussion. I wonder whether nasal oxygen was used and if the canula caused damage to the nose. It cold also have followed H. zoster. This is the picture that can be seen with Trigeminal Trophic Syndrome, a rare disorder that is thought to be traumatic in origin. Has anyone seen a similar picture and what are your thoughts.?
This is a good abstract:
Laryngoscope. 1988 Dec;98(12):1330-3.
Trigeminal trophic syndrome.
Arasi R, McKay M, Grist WJ.
Department of Dermatology, Emory University School of Medicine, Atlanta, GA.
Trigeminal trophic syndrome is an unusual condition also known as trigeminal
neurotrophic ulceration or trigeminal neuropathy with nasal ulceration. The
diagnosis is suggested when ulceration of the face, especially of the ala nasi,
occurs in a dermatome of the trigeminal nerve that has been rendered anesthetic
by a surgical or other process involving the trigeminal nerve or its central
sensory connections. A history of paresthesias and self-induced trauma to the
area further support the diagnosis. Neurological deficits causing trigeminal
trophic syndrome may result from surgical trigeminal ablation, vascular
disorders and infarction of the brainstem, acoustic neuroma, postencephalitic
parkinsonism, and syringobulbia. The following etiologies of nasal ulceration
should be excluded: postsurgical herpetic reactivation and ulceration, syphilis,
leishmaniasis, leprous trigeminal neuritis, yaws, blastomycosis,
paracoccidioidomycosis, lethal midline granuloma, pyoderma gangrenosum,
Wegener's granulomatosis, and basal cell carcinoma. In the case reported here,
the diagnosis of TTS was made primarily as a result of previous experience with
the syndrome, underscoring the importance of physician recognition of this
unusual disorder.