The patient is an 11 year-old girl with a one-year history
of a dermatitis in the right retroauricular sulcus. She has a history of an eczematous
eruption on her thighs. She was prescribed mupirocin and betamethasone
valerate ointmens. They both caused
burning and pruritus and she refused to use them. There is a history of a vaginal dermatitis a
year or so ago, which was successfully treated with topical corticosteroids.
O/E: There is
erythema, crusting and mild fissuring in the above-mentioned area. The left retorauricular area is mildly
affected. Presently there are no
findings of atopic dermatitis in the usual areas.
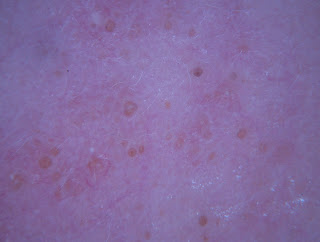
Clinical Image:
Lab: Wound culture
was positive for 3+ Staph aureus and 3+ Group B Strep.
Diagnosis:
Retroauricular dermatitis.
We prescribed cephalexin 250 mg q.i.d. and a small amount of
Vaseline for the dryness and fissuring.
Patch testing will be recommended if there are further symptoms
suggestive of contact dermatitis.
Comments:
Retroauricular dermatitis, also called "infra-auricular fissures," appears to be an under-reported entity. Although it is common in atopic dermatitis, there have been few articles about it. I see a few cases a year and the vast
majority yield coagulase positive Staph aureus and occasionally strep when
cultured. Most respond quickly to mupirocin ointment and a low to moderate strength topical
steroid. This patient’s symptoms make
her an outlier. In addition, she has no findings of atopic dermatitis at this time.
Do any of you have
thoughts on this entity? The take home message here is that, as with atopic dermatitis, these lesions are frequently colonized with Staph aureus.
References
1. Infra-auricular fissures in atopic dermatitis.
Tada J, et. al. Acta Derm Venereol. 1994 Mar;74(2):129-31.
Abstract: Retro-auricular
or auricular dermatitis in atopic dermatitis (AD) is common and important for
the diagnosis of AD in infancy and even in adulthood. Particularly,
"infra-auricular fissures", acute eczematous changes like fissures at
the adhesive junction of ear lobes, seem to be prominent features for the
diagnosis of AD. Of 137 patients with AD, 81.8% showed present or past
existence of infra-auricular fissures, but only one of the 30 controls. Of the
46 patients with severe AD, 98% had infra-auricular fissures, compared to 74%
in those with moderate and mild AD. Our findings suggest that infra-auricular
fissures are important for the diagnosis of AD and should be cited in a list of
criteria for the diagnosis of AD.
2. Streptococcal perianal disease in children. Kokx NP,
Comstock JA, Facklam RR.
Pediatrics.
1987 Nov;80(5):659-63.
PubMed Link.
3. Psoriasis inversa: A separate identity or a variant of
psoriasis vulgaris?
Omland SH, Gniadecki R. Clin Dermatol. 2015
Jul-Aug;33(4):456-61.
Abstract: Psoriasis
is a chronic skin disorder affecting approximately 2% of the European and
American population. The most common form of psoriasis is the chronic plaque
type. Inverse psoriasis, also named flexural or intertriginous psoriasis, is
not considered a separate disease entity but rather a special site of
involvement of plaque psoriasis, characterized by its localization to
inverse/intertriginous/flexural body sites. We review current evidence and
establish whether inverse psoriasis is a separate disease entity based on
characteristics in terms of epidemiology, pathogenesis, clinical and histologic
presentation, microbiology, and treatment.
.