Abstract: 61 yo man with 4 - 5 year hx of a tumor on foot.
HPI: The patient is a healthy 61 year old man with a 4 - 5 year history of a slowly growing lesion on the plantar aspect of his right foot. On a recent trip to Jamaica it bled, leading him to consult a podiatrist who astutely did a biopsy. The patient has sarcoidosis which has been treated with weekly i.m. methotrexate for the past two years. (I do not know the dose byt presume it is around 15 mg).
O/E: 2 x 1 cm flesh-colored nodule. Crust in photo is from punch biopsy. Remainder of cutaneous exam unremarkable. No palpable regional lymph nodes. Dermatoscopic exam was not rewarding.
Photo:Lab: Mild leucopenia 3700. Otherwise all chemistries and LDH normal
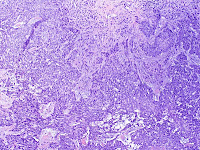
Pathology: ALM 3.68 (at least) mm thick, (at least) Level IV.
Tumor thickness may be deeper tumor is present at the base of the specimen.
Regression: Not Present
Vascular/lymphatic invasion: Not identified
Mitotic Activity: 7/10 HPF
Tumor Infiltrating Lymphocytes: Non-brisk
Vertical Growth Phase: Present
Discussion: Although this tumor is called "acral lentiginous melanoma" it clearly is a nodular lesion. Might it better be called "acral nodular melanoma?" The patient will need staging and the, depending on findings of staging studies, a wide-local excision with lymph node mapping . He is being referred to the melanoma clinic at Dartmouth Mary Hitchcock Medical Center.
This is an amelanotic acral melanoma that has been present 4 - 5 years by history. Amelanotic acral melanoma are scary lesions as clinically and dermoscopically they do not appear to be worrisome.
It is well-recognized that these can fool practitioners, as they are only rarely seen even by dermatologists and a high index of suspicion is needed. The podiatrist who saw the patient was astute to biopsy the lesion on his first visit.
References:1. Acral lentiginous melanoma: a clinicoprognostic study of 126 cases.Phan A, Touzet S, Dalle S, Ronger-Savlé S, Balme B, Thomas L.
Br J Dermatol. 2006 Sep;155(3):561-9.
Department of Dermatology, Hôtel Dieu, Claude Bernard University, 69288 Lyon cedex 02, France.
Abstract:
BACKGROUND: Although the histopathological subtype of melanoma has not been clearly proven to carry independent prognostic significance, acral lentiginous melanoma (ALM) seems to confer a poorer prognosis mainly because disease is often more advanced at the time of diagnosis.
OBJECTIVES: To investigate the distinctive epidemiological and clinical characteristics of ALM, a peculiar histological entity, and to identify prognostic factors.
METHODS: We performed a register-based review of cases from a single large referral centre, the University Hospital Department of Dermatology, Lyons, France. We reviewed patient demographics, the initial presentation of the lesion, and clinical outcome. ALM-specific and disease-free survival were estimated using the KaplanMeier method and compared using the log-rank test. A Cox model was used to identify prognostic factors.
RESULTS: One hundred and twenty-six patients were identified as having histopathology-proven ALM in our melanoma patient register from 1996 to 2004. There were 46 (37%) subungual ALM and 80 (63%) ALM on soles, palms and nonvolar sites. The mean age at diagnosis was 63 years. There were 44 (35%) men and 82 (65%) women, sex ratio M/F 1 : 1.86. The mean Breslow thickness was 2.51 mm (range: in situ to 20 mm). There was no evidence of overexposure to ultraviolet radiation, nor was there found a predisposing genetic trait. Only 16 (13%) patients recalled a history of trauma. Thirty-four ALM (28%) were unpigmented. The median ALM-specific and disease-free survival were 13.5 and 10.1 years, respectively. The 5-year survival rate was 76%. Multivariate analysis identified tumour thickness, male gender and amelanosis as independent clinical prognostic factors for both ALM-specific and disease-free survival.
CONCLUSIONS: Our study provides specific information on the clinical characteristics and outcome of this uncommon histological subtype of melanoma. However, the pathogenesis remains unknown. Breslow thickness, male gender and amelanosis were significantly associated with a poorer prognosis.
2. Acral lentiginous melanoma mimicking benign disease: the Emory experience.Soon SL, Solomon AR Jr, Papadopoulos D, Murray DR, McAlpine B, Washington CV.
J Am Acad Dermatol. 2003 Feb;48(2):183-8.
Abstract
BACKGROUND: Plantar and subungual melanoma exhibits a higher misdiagnosis rate relative to other anatomic sites. Misdiagnosis and delay in diagnosis are statistically associated with poorer patient outcome. Awareness of atypical presentations of acral melanoma may, thus, be important to decrease misdiagnosis rates and improve patient outcome.
METHODS: We conducted a retrospective case review of plantar or lower-extremity subungual melanoma performed at Winship Cancer Center, a tertiary care, referral center affiliated with Emory University, between 1985 and 2001.
RESULTS: A total of 53 cases of plantar or lower-extremity subungual melanoma were identified. Of 53 cases with a final diagnosis of melanoma, 18 were initially misdiagnosed. Misdiagnoses included wart, callous, fungal disorder, foreign body, crusty lesion, sweat gland condition, blister, nonhealing wound, mole, keratoacanthoma, subungual hematoma, onychomycosis, ingrown toenail, and defective/infected toenail. Of the 18 misdiagnosed cases, 9 were clinically amelanotic.
CONCLUSION: Awareness that amelanotic variants of acral melanoma may assume the morphology of benign hyperkeratotic dermatoses may increase the rate of correct diagnosis and improve patient outcome.