Recently I saw this 40 year old woman who presented with severe blisters and erosions. It started about 3 weeks ago and spread quite rapidly from the chest to the face and extremities. Now her mouth is also involved.
Exam: generalised bulla, majority are flaccid type. Erosions extensive with crusts esp anterior chest wall. Superficial erosions on the lower lips. Nikolysky sign positive.


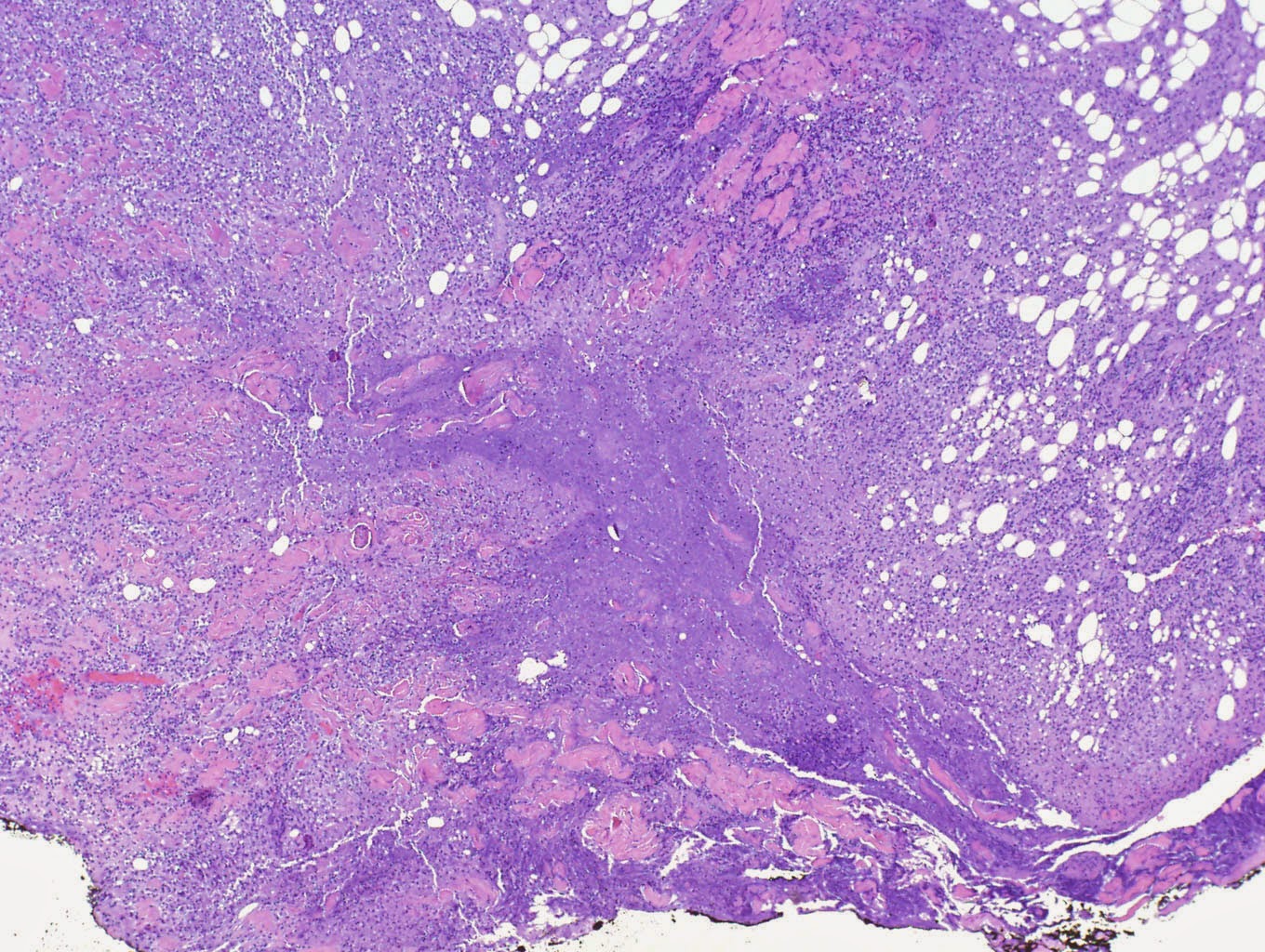
Skin biopsy: Section shows skin composed of epidermis and dermis. A suprabasal bulla
containing acantholytic cells is seen. In areas, a tombstone appearance
is seen. Infiltrates of eosinophils and lymphocytes are seen in the
dermis.
Pemphigus vulgaris
Blood counts and biochemistry are normal.
She was treated as outpatient. I have started her on oral prednisolone 40mg daily. Added oral antibiotics cefuroxime 250mg bd. Skin dressing with KMNO4 wet compress followed by fusidin/hydrocort cream bd. Keep skin roof intact.
Questions:
- I do not have IF facilities. Will this lack of facilities affect her prognosis?
- what kind of skin dressing would you use?
- would you use steroid sparing agent like mycophenolate, MTX , azathioprine or ritazulimab at this juncture?
Thanks for your help. Your comments are greatly valued.
References:
Cochrane reviews: Interventions for pemphigus vulgaris and pemphigus foliaceus
Published Online:
15 April 2009
This review of clinical trials aimed to find out which is the most effective and safest treatment option for pemphigus vulgaris and pemphigus foliaceus.
Pemphigus vulgaris and pemphigus foliaceus are rare diseases characterised by fragile blisters and sores on the skin and mucosa. They are auto-immune diseases which are caused by the body making an antibody against the person's own skin. These diseases are chronic and are not currently curable. Pemphigus vulgaris and foliaceus are managed with drugs which suppress the immune system. The aim of treatment is to suppress blister formation. Systemic glucocorticoids are the cornerstone of management in pemphigus, however adjuvant immunosuppressive and anti-inflammatory agents are commonly used. There are many treatments available, however it is not known which is the most effective or safest treatment option, or which is the best combination.
This review included data from 11 clinical trials involving 404 participants. The studies had very small numbers of participants, so can provide only limited information. Ten different active treatments were studied, including prednisolone, pulsed oral dexamethasone, azathioprine, cyclophosphamide, cyclosporine, dapsone, mycophenolate, plasma exchange, topical epidermal growth factor and traditional Chinese medicine.
This review found insufficient information to conclude which is the most effective and safest treatment plan. We found that mycophenolate mofetil appears to be more effective than azathioprine in controlling disease, although no difference was seen in remission. We found that taking azathioprine and cyclophosphamide decreased the amount of glucocorticoids required. Topical epidermal growth factor decreased time required for lesions to heal by 6 days (median). We found no difference in withdrawal due to adverse events in any study, although differing adverse event profiles were observed for each intervention. We were not able to conclude which treatments are superior overall.
Multiple treatments are available for pemphigus vulgaris and pemphigus foliaceus and there is a variation in dosage plan and combination of drugs used, which makes choice of treatment schedule complex. In addition, response to treatment can vary between individuals. Treatments need to be chosen after careful consideration of the potential benefits and side effects, in the context of the individual's other medical conditions. This review found insufficient information to conclude which is the most effective and safest treatment regimen. Further studies are required to determine the optimal treatment regimen, especially to assess the optimal glucocorticoid dose, the role of adjuvant immunosuppressive medications, and long-term adverse events to improve harm:benefit analyses.