The patient is a 35 year old man who has had a right-sided eyelid dermatitis for around eight months. He was given a moderate strength topical steroid for this by his primary care physician and has been using it off and on since. When the process flares, he applies it again.
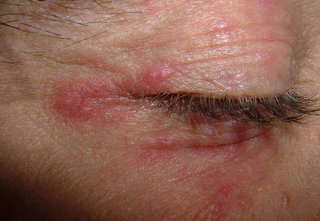
There are discrete erythematous papules around the upper and lower lids on the right side. The left eyelids are clear.
The clinical picture suggests a steroid-induced periocular acne.
Treatment: cold tap water compresses, doxycycline 100 mg. bid. Is there a role for tacrolimus ointment?
Affected Right Eye
Normal Left Eye

References:
1.
J Am Acad Dermatol. 1999 Sep;41(3 Pt 1):435-42.
Eyelid dermatitis to red face syndrome to cure: clinical experience in 100
cases.
Rapaport MJ, Rapaport V.
A retrospective review of all eyelid dermatitis patients seen over an 18-year
period revealed a large subgroup of patients who had, as the basis for their
ongoing problem, an addiction to the use of topical or systemic corticosteroids.
This group of 100 patients often sought many consultations with various
physicians. Unrelenting eyelid or facial dermatitis often resulted in the use of
increasing amounts of corticosteroids for longer periods of time. Soon the skin
became addicted. Once the work-up ruled out other causes, the remedy for the
problem was absolute total cessation of corticosteroid usage. This article
describes the typical history of the problem, the evaluation of these patients,
and the distinctive pattern of flaring erythema that ensued when the
corticosteroids were ceased. We stress the absolute necessity of total cessation
of corticosteroid use as the only treatment for corticosteroid addiction. We
also demonstrate that no additional therapy or further consultations were
necessary once remission was obtained after topical corticosteroid abuse was
stopped.
2.
West J Med. 2001 Jun;174(6):383-4.
"Tortured tube" sign.
Fowler KP, Elpern DJ.
Medical University of South Carolina Charleston, SC. Williamstown, MA, USA.
(This is available as full text - go to http://www.pubmed.gov find this article and you can see the full text version. This was a patient Dr. Fowler saw in my office 5 years ago.)