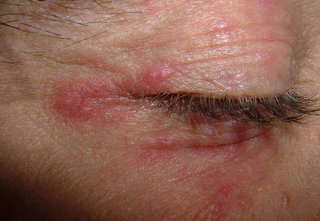
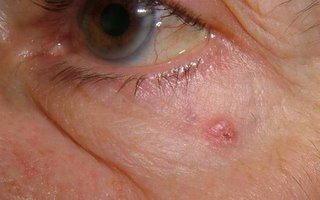
This 20 yo college student presented in consultation for removal of a congenital nevus.
The lesion is located just distal to her left knee. She's been embarrassed about this since childhood and for the past six or seven years won't let anyone see it. Indeed she covers it at all times with bandaids.
The lesion measures 5.2 cm in diameter.
I have referred her to a surgeon for removal since I think that's better than psychotherapy. To minimize the scar it may need staged excision.
The young woman appears normal in all other respects - she is very upset about the lesion and the questions she gets about it.
I wonder if this has been reported. I would hardly call this Body Dysmprphic Syndrome.
Your thoughts are appreciatged.
Not much written about this area -- here's a ref that may touch on it:
Congenital melanocytic nevi. Evaluation and management.
Marghoob AA., Dermatol Clin. 2002 Oct;20(4):607-16, viii.
Department of Medicine, Dermatology Division, Memorial Sloan-Kettering Cancer Center, 1275 York Avenue, New York, NY 10021, USA. marghooa@mskcc.org
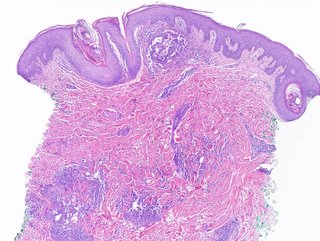
This article discusses the care of patients with CMN, who often require
a multidisciplinary approach involving pediatricians, family physicians,
internists, dermatologists, psychologists, plastic surgeons,
neurologists, and radiologists. The cosmetic and psychosocial issues,
combined with the knowledge of the increased risk of developing
melanoma or NCM, is a huge burden that many of these patients
and their families have to carry. This article describes the importance
for physicians to help these patients and families come to terms
with these issues, as well as remind their patients and their family
members that although melanoma, NCM, or other complications can
develop, most affected individuals do not develop any complications.
The article mentions that there are many healthy, happy, functional
adults with large, small, and multiple CMN alive today.