Dear Colleagues,
Please help me with a 4 year-old lad who was referred today by his GP for genital warts. A court-appointed foster parent brought him in for evaluation. His 21 year-old mother left him recently with relatives. She is an inattentive parent with an alcohol and possibly a drug problem. The child was in pre-school but was suspended a few days ago because he was using sexually explicit language, being physically abusive to his peers, discussing French kissing and saying he was going to shoot himself.
The exam showed a quiet, calm and health 4 year-old. The only findings were lobulated and verrucous flesh-coloured papules grouped on the shaft of the penis. There were no bruises or evidence of trauma.
Diagnosis: Condyloma acuminata.
Photos were removed at advice of a pediatrician. Apparently, FBI may moniter some sites. Gets my Canadian soul anxious!
Discussion:
Although genital warts in children can occur in the absence of child sexual abuse, this case is suspicious. The child's broken home, the fact that he has been left with numerous teenage girls as baby sitters, his sexually explicit language, his antisocial behavior and language all are red flags for a child at risk.
Here, in Nova Scotia, we are mandated to report such children to the authorities. I would like to ask wo questions:
1) Your opinion as to whether reporting this child is appropriate.
2) How should he be treated?
a) electrosurgery under general anesthesia
b) cryo therapy
c) imiquimod or podophyllin.
Your thoughts and comments are most welcome.
Hamish Dunwoodie, M.D. FRCPC - Paediatrics
Moncton, NS, Canada
This is a rapid publication site that replaces Virtual Grand Rounds in Dermatology (vgrd.org). Please join and feel free to post cases. You can share the URL with friends. Since 2000, VGRD has been a valuable means to share cases in real time from one's home or office. "AND GLADLY WOLDE HE LERNE AND GLADLY TECHE" has served as an enduring and inspirational motto. For more information, see the "About Page."
Saturday, December 30, 2006
Thursday, December 28, 2006
Unusual Case
This 53 yo man presented with a three week history of a pustular eruption on the left small finger. It began as a papule and slowly enlarged.
History reveals that he has a farm with 500 sheep. He has also been exposed to cats and dressed a deer around a month ago.
Diagnostic tests were done.


Follow-up: The KOH prep was positive. The fungal culture is positive at ten days. Thus, this is inflammatory tinea manus. Await fungal culture for typing of dermatophyte. Resolved with dilute Clorox soaks and 2% ketoconazole cream in one week.
12 days after initial visit.

History reveals that he has a farm with 500 sheep. He has also been exposed to cats and dressed a deer around a month ago.
Diagnostic tests were done.


Follow-up: The KOH prep was positive. The fungal culture is positive at ten days. Thus, this is inflammatory tinea manus. Await fungal culture for typing of dermatophyte. Resolved with dilute Clorox soaks and 2% ketoconazole cream in one week.
12 days after initial visit.

Saturday, December 16, 2006
Unilateral Bullae
History
The patient is a 28 yo man referred on a walk-in basis with an eight month history of a bullous eruption on the dorsum of his left hand. He gets one or two painless lesions a month. No history was sent over with the patient and he is a poor historian. His medications include Welbutrin, Clozeril and Soma (carisprodol/aspirin)
Exam:
The only findings are on the dorsum of the left hand. Here, there is a hemorrhagic bulla, a vesicle and areas of mild erythema at sites of previous lesions.


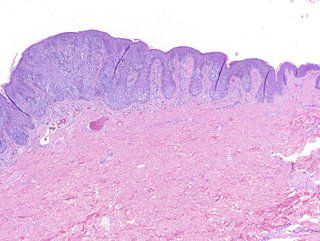
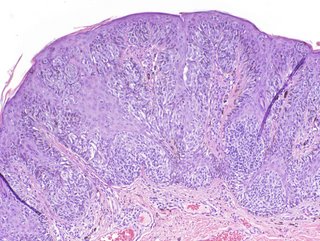
Biopsy:
I suspect fixed drug or pseudoporphyria cutanea tarda. I biopsied the small papule and the edge of the bullae and made a follow-up appointment.
Path Report:
A subepidermal separation, individually necrotic keratinocytes , and a sparse superficial perivascular lymphocytic infiltrate with occasional neutrophils .
NOTE : (A and B). Amphophilic globular material is seen deposited in the dermis and around blood vessels in both specimens. This material is P.A.S. stain positive, and stains negative for amyloid and elastic tissue. The differential diagnosis could include porphyria cutanea tarda , although this is usually less inflammatory. A subepidermal autoimmune bullous disorder could also be considered. An additional biopsy for direct immunofluorescence may be of help.
Laboratory Studiess:
CBC normal, LFTs normal, ferritin normal. Hep B and C negative, All urinary porphyrins well within normal levels. Uroporphyrin: 9.6 ug (nl < 30.0) Coproporphyrin 40 ug (normal < 65/24 hr)
Discussion: This is likely pseudoporphyria cutanea tarda. A similar case has been reported. Your comments are welcomed.
The patient is a 28 yo man referred on a walk-in basis with an eight month history of a bullous eruption on the dorsum of his left hand. He gets one or two painless lesions a month. No history was sent over with the patient and he is a poor historian. His medications include Welbutrin, Clozeril and Soma (carisprodol/aspirin)
Exam:
The only findings are on the dorsum of the left hand. Here, there is a hemorrhagic bulla, a vesicle and areas of mild erythema at sites of previous lesions.


Biopsy:
I suspect fixed drug or pseudoporphyria cutanea tarda. I biopsied the small papule and the edge of the bullae and made a follow-up appointment.
Path Report:
A subepidermal separation, individually necrotic keratinocytes , and a sparse superficial perivascular lymphocytic infiltrate with occasional neutrophils .
NOTE : (A and B). Amphophilic globular material is seen deposited in the dermis and around blood vessels in both specimens. This material is P.A.S. stain positive, and stains negative for amyloid and elastic tissue. The differential diagnosis could include porphyria cutanea tarda , although this is usually less inflammatory. A subepidermal autoimmune bullous disorder could also be considered. An additional biopsy for direct immunofluorescence may be of help.
Laboratory Studiess:
CBC normal, LFTs normal, ferritin normal. Hep B and C negative, All urinary porphyrins well within normal levels. Uroporphyrin: 9.6 ug (nl < 30.0) Coproporphyrin 40 ug (normal < 65/24 hr)
Discussion: This is likely pseudoporphyria cutanea tarda. A similar case has been reported. Your comments are welcomed.
Sunday, November 05, 2006
Mystery Rash in Runners
The Williams Cross Country running team went to a meet on the Connecticut shore on Saturday, October 28. There had been a big storm the previous day. The course took them through brackish water sometimes thigh deep. Within a 24 - 48 hours, around half of the runners had developed intensely pruritic lesions on arms and legs. The vast majority of the lesions were on exposed skin. The primary lesion appears to be a juicy papule or a clear vesicle. Some of these have crusted over in a few days. The lesions are discrete. They do not have the linear pattern characteristic of phytocontact dermatitis from a plant such as poison ivy. The pictures were taken of the legs of an 18 yo woman and a 21 yo man. The lesions were quite similar.


It's likely that this is from something dispersed in the brackish water they ran through. Runners from other schools were affected as well. About 50 runners from Williams College developed the eruption.
The possibilities include:
Atypical plant contact dermatitis (Some plant toxin such as urushiol churned up by the storm and floating in the water.)
Jellyfish nematocysts free floating after the storm and blown in
Bird schistosomes -- this is severe for that.
Bacterial infection (a culture was taken from one student and results were not specific)
Do you have other thoughts? What is your opinion?
Solution: The Cross Country course was redirected after the storm. A new path was cut though brush to circumvent a brackish area. It is likely that the new path went through poison ivy. The appearance of the rash 24 - 48 hours after exposure in the majority of runners and the quality of the itch suggests rhus contact dermatitis.


It's likely that this is from something dispersed in the brackish water they ran through. Runners from other schools were affected as well. About 50 runners from Williams College developed the eruption.
The possibilities include:
Atypical plant contact dermatitis (Some plant toxin such as urushiol churned up by the storm and floating in the water.)
Jellyfish nematocysts free floating after the storm and blown in
Bird schistosomes -- this is severe for that.
Bacterial infection (a culture was taken from one student and results were not specific)
Do you have other thoughts? What is your opinion?
Solution: The Cross Country course was redirected after the storm. A new path was cut though brush to circumvent a brackish area. It is likely that the new path went through poison ivy. The appearance of the rash 24 - 48 hours after exposure in the majority of runners and the quality of the itch suggests rhus contact dermatitis.
Sunday, October 22, 2006
Teenager with a Red Nose


This 14 year-old girl has had a red nose for the past two years. It followed as severe sunburn. Her nose never looks normal. Occasionally, there are small cysts with bleeding and purulent drainage.
I have seen this picture occasionally in teenagers. It looks like a rosacea variant. I'd also consider demodex.
Your suggestions are anticipated and will be welcome.
Sunday, September 24, 2006
30 year old woman with changing mole

This 30 yo woman has noticed an enlarging pigmented lesion in her right axilla for almost a year. Her mother, a registered nurse, asked her to see a dermatologist. Her husband did not notice it.
The patient has Type II skin. The general cutaneous exam was unremarkable save for a 1.2 cm in diameter barely elevated plaque. There is a play of pigment and outline is irregular.
An excisional biopsy was performed.
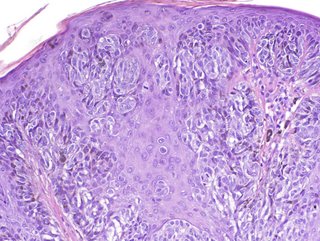
Pathology: Malignant melanoma in situ , superficial spreading type. (Read by H. Byers of BU Skin Path who took photomicrographs) "The specimen exhibits a marked nested and lentiginous melanocytic proliferation with large severely atypical epithelioid cells. There is irregular nesting, focal confluent lentiginous melanocytic proliferation and cellular dyshesion."
She is scheduled for a wider excision, 0.5 cm on either side. No further work-up other than regular follow-up visits.
Your thoughts are appreciated.
Wednesday, September 20, 2006
Positive Band Aid Sign
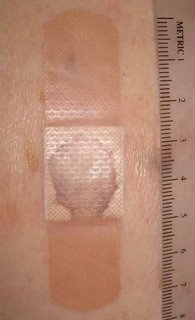
Most dermatologists know about the "positive band aid sign." To me, it means a skin cancer has been lurking there for a while.
This 82 yo man came in with a one year history of a "sore" on his back. The drainage stained his shirt. When the band aid was removed, there was a one cm in diameter clean friable tumor, most likely a basal cell.
The lesion was shave biopsied and desicated and curetted. I'll affix a copy of the biopsy report when I get it.
How many of you use the term "Positive band Aid Sign?"
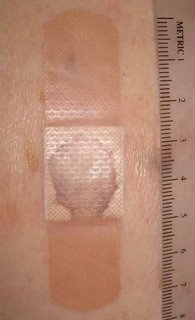

This 82 yo man came in with a one year history of a "sore" on his back. The drainage stained his shirt. When the band aid was removed, there was a one cm in diameter clean friable tumor, most likely a basal cell.
The lesion was shave biopsied and desicated and curetted. I'll affix a copy of the biopsy report when I get it.
How many of you use the term "Positive band Aid Sign?"

Wednesday, August 30, 2006
BCC of Eyelid
This 43 yo man has a one year history of a lesion of the left lower lid. It measures 8 mm in diameter.
Biopsy from "X" confirms "nodular BCC."
Question: What is best therapy?
1) Mohs
2) Mohs + closure by ophthalmic plastic surgeon
3) Ophthalmic plastic surgeon handle all
4) Another approach
Cada vendador allabe sus agujas.
Every peddler praises his needles.

Biopsy from "X" confirms "nodular BCC."
Question: What is best therapy?
1) Mohs
2) Mohs + closure by ophthalmic plastic surgeon
3) Ophthalmic plastic surgeon handle all
4) Another approach
Cada vendador allabe sus agujas.
Every peddler praises his needles.

Wednesday, August 02, 2006
Therapeutic Question
The patient is an 83 year-old woman with a two year history of a lesion on the nose.
Clinically, this is a basal cell. My question is what you would recommend as therapy and why?
1) Micrographic surgery with forehead advancement flap.*
2) Micrographic surgery with graft or allowed to heal by secondary intention.
3) Radiotherapy
3) Other


* Repair of defects on nasal sebaceous skin.
Dzubow LM.
Department of Dermatology, University of Pennsylvania Health System, Philadelphia, 19085, USA. leonarddzubow@comcast.net
BACKGROUND: Reconstructive procedures performed on sebaceous nasal skin are prone to partial flap necrosis, scar spread and inversion, and tissue mismatch. An ideal repair would optimize vascular integrity, minimize closure tension, and use adjacent tissue. OBJECTIVE: The purpose of this article is to describe a flap design and dynamics that permit satisfactory reconstruction of small- to medium-sized defects on nasal sebaceous tissue. METHODS: A modified advancement flap is described that may be used on central and off-midline defects of the nasal tip. RESULTS: Use of the modified advancement flap resulted in good cosmetic results with few adverse postsurgical events. CONCLUSIONS: The modified advancement flap satisfies the requirements of a hardy blood supply, minimization of closure tension, and use of adjacent tissue. The surgical results are predictable and rarely associated with complications.
Clinically, this is a basal cell. My question is what you would recommend as therapy and why?
1) Micrographic surgery with forehead advancement flap.*
2) Micrographic surgery with graft or allowed to heal by secondary intention.
3) Radiotherapy
3) Other


* Repair of defects on nasal sebaceous skin.
Dzubow LM.
Department of Dermatology, University of Pennsylvania Health System, Philadelphia, 19085, USA. leonarddzubow@comcast.net
BACKGROUND: Reconstructive procedures performed on sebaceous nasal skin are prone to partial flap necrosis, scar spread and inversion, and tissue mismatch. An ideal repair would optimize vascular integrity, minimize closure tension, and use adjacent tissue. OBJECTIVE: The purpose of this article is to describe a flap design and dynamics that permit satisfactory reconstruction of small- to medium-sized defects on nasal sebaceous tissue. METHODS: A modified advancement flap is described that may be used on central and off-midline defects of the nasal tip. RESULTS: Use of the modified advancement flap resulted in good cosmetic results with few adverse postsurgical events. CONCLUSIONS: The modified advancement flap satisfies the requirements of a hardy blood supply, minimization of closure tension, and use of adjacent tissue. The surgical results are predictable and rarely associated with complications.
Wednesday, July 26, 2006
An Incidental Finding


The patient is an 85 yo man who presented for generalized pruritus which has been present for two years. He has a history of prostate cancer and gastrointestinal bleeding. He's had a few transfusions over the past year or so and was concerned that they caused his itching.
He did not complain about his nose. I asked about it and he and his daughter gave this history: Three years ago he was hospitalized for pneumonia. He delvelped an inflammation of the ala nasi and was told it was "shingles." Biopsies were done and ruled out cancer. The left ala nasi was destroyed and this is how he healed.
Discussion. I wonder whether nasal oxygen was used and if the canula caused damage to the nose. It cold also have followed H. zoster. This is the picture that can be seen with Trigeminal Trophic Syndrome, a rare disorder that is thought to be traumatic in origin. Has anyone seen a similar picture and what are your thoughts.?
This is a good abstract:
Laryngoscope. 1988 Dec;98(12):1330-3.
Trigeminal trophic syndrome.
Arasi R, McKay M, Grist WJ.
Department of Dermatology, Emory University School of Medicine, Atlanta, GA.
Trigeminal trophic syndrome is an unusual condition also known as trigeminal
neurotrophic ulceration or trigeminal neuropathy with nasal ulceration. The
diagnosis is suggested when ulceration of the face, especially of the ala nasi,
occurs in a dermatome of the trigeminal nerve that has been rendered anesthetic
by a surgical or other process involving the trigeminal nerve or its central
sensory connections. A history of paresthesias and self-induced trauma to the
area further support the diagnosis. Neurological deficits causing trigeminal
trophic syndrome may result from surgical trigeminal ablation, vascular
disorders and infarction of the brainstem, acoustic neuroma, postencephalitic
parkinsonism, and syringobulbia. The following etiologies of nasal ulceration
should be excluded: postsurgical herpetic reactivation and ulceration, syphilis,
leishmaniasis, leprous trigeminal neuritis, yaws, blastomycosis,
paracoccidioidomycosis, lethal midline granuloma, pyoderma gangrenosum,
Wegener's granulomatosis, and basal cell carcinoma. In the case reported here,
the diagnosis of TTS was made primarily as a result of previous experience with
the syndrome, underscoring the importance of physician recognition of this
unusual disorder.
Monday, July 24, 2006
Tale of Two Lesions
I saw these two patients today. Your comments are most welcome. Path reports will be affixed when available.
1) 69 yo man with 1.5 month history of lesion right pinna. The lesion is slowly growing. The patient's son, a family doctor, asked him to make an appointment. This is a subtle lesion that could be a lentigo or a lentigo maligna. Two representative areas were biopsied.

2) A 55 year-old priest whose parishioner noted a lesion on his left arm and asked him to see a doctor about it. He's been aware of this lesion for 3 months. It appears that the darkly pigmented papule began in a lentigo. I favor a diagnosis of melanoma here but this could be a seborrheic keratosis. An excisional biopsy of raised and macular portions was performed and based on pathology I will recommend further therapy.


1) 69 yo man with 1.5 month history of lesion right pinna. The lesion is slowly growing. The patient's son, a family doctor, asked him to make an appointment. This is a subtle lesion that could be a lentigo or a lentigo maligna. Two representative areas were biopsied.

2) A 55 year-old priest whose parishioner noted a lesion on his left arm and asked him to see a doctor about it. He's been aware of this lesion for 3 months. It appears that the darkly pigmented papule began in a lentigo. I favor a diagnosis of melanoma here but this could be a seborrheic keratosis. An excisional biopsy of raised and macular portions was performed and based on pathology I will recommend further therapy.


Thursday, July 20, 2006
Hypopigmentation in atopic dermatitis
This is a 7-year-old boy who developed multiple patches of hypopigmentation on the dorsum of the hands for 3 years. He had a history of atopic dermatitis and had severe eczema of the hands prior to development of the hypopigmentation on the hands. According to the mother, he had secondary infection with crusts formation on the hands. The lesions were patchy hypopigmented macules mainly on the dorsum of the hands and feet. There were no family history of similar pigmentation. Wood's lamp examination however showed accentuation of the hypopigmented lesions.
Based on history this is most likely post inflammatory. Other differential considered includes vitiligo. Vitiligo is probably unlikely in this patient as the hypopigmentation developed after he had eczema with secondary infection of the hands and feet.
Any suggestions for this hypopigmentation? Would UVB or tacrolimus ointment help?
Thanks for your comments.



Based on history this is most likely post inflammatory. Other differential considered includes vitiligo. Vitiligo is probably unlikely in this patient as the hypopigmentation developed after he had eczema with secondary infection of the hands and feet.
Any suggestions for this hypopigmentation? Would UVB or tacrolimus ointment help?
Thanks for your comments.



Wednesday, July 12, 2006
A Case from New Brunswick
A friend from coastal New Brunswick sent this interesting case:
Dear Dr. Elpern,
The patient is a 91 year-old working lobsterman who was sent in by his GP for evaluation of a large fungating tumour on his left temple. By history, the lesion has been present for 15 years but has only really increased in size in the past 18 months. He's in vigourous good health otherwise.
On close examination, the tumour was found to be on a stalk. It's surface measured around 5 cm in diameter, whilst the pedicle was 9 mm in diameter.
After cleaning the area, I administered local anesthesia with lidocaine and epinephrine and snipped it off. I dissicated the base and applied a dressing.
I may follow-up with imiquimod (as recommended by a dermatologic friend) or may excise the defect secondarily.
We occasionally see dramatic tumours like this is watermen. They are a stoic lot.
I wonder, do your colleagues have any suggestions? I will post the path report when it is ready.
Cheers,
Dr. Hamish Dunwoodie, FRCSC
General Surgeon
Moncton, NB, Canada



Dear Dr. Elpern,
The patient is a 91 year-old working lobsterman who was sent in by his GP for evaluation of a large fungating tumour on his left temple. By history, the lesion has been present for 15 years but has only really increased in size in the past 18 months. He's in vigourous good health otherwise.
On close examination, the tumour was found to be on a stalk. It's surface measured around 5 cm in diameter, whilst the pedicle was 9 mm in diameter.
After cleaning the area, I administered local anesthesia with lidocaine and epinephrine and snipped it off. I dissicated the base and applied a dressing.
I may follow-up with imiquimod (as recommended by a dermatologic friend) or may excise the defect secondarily.
We occasionally see dramatic tumours like this is watermen. They are a stoic lot.
I wonder, do your colleagues have any suggestions? I will post the path report when it is ready.
Cheers,
Dr. Hamish Dunwoodie, FRCSC
General Surgeon
Moncton, NB, Canada



Friday, July 07, 2006
Probably Lyme
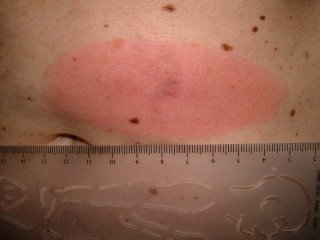
The patient is a 56 year old man in good general health.
Six days ago, he developed an erythematous papule on the left abdomen.
Over the past week, this has grown into an oval 10 centimeter pruritic erythematous plaque.
This is a solitary lesion and the remainder of the cutaneous exam is unremarkable.
There is no history of tick bite, but this is an endemic area and the patient has an outdoor life-style.
I suspect this is Lyme Disease and that it is too early for serology to be helpful.
After discussion with the patient, he was started on doxycycline 100 mg bid.
(For interest, please see case of June 20th)
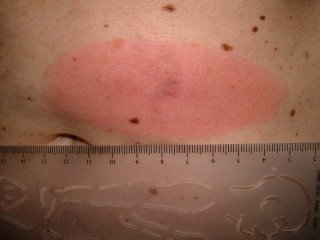
Six days ago, he developed an erythematous papule on the left abdomen.
Over the past week, this has grown into an oval 10 centimeter pruritic erythematous plaque.
This is a solitary lesion and the remainder of the cutaneous exam is unremarkable.
There is no history of tick bite, but this is an endemic area and the patient has an outdoor life-style.
I suspect this is Lyme Disease and that it is too early for serology to be helpful.
After discussion with the patient, he was started on doxycycline 100 mg bid.
(For interest, please see case of June 20th)
Wednesday, June 28, 2006
Eye Lash Alopecia
The patient is an eight year old girl who has had a dermatitis of her eyelid margins off an on for around a year. She gets crusted areas which itch and her mother feels she plucks her eyelashes. On the day of the visit the lids looked quiet, but there was definite loss of some eyelashes. There is some evidence of broken lashes.
Question:
Is this eyelash trichotillomania or isolated alopecia areata of the eyelashes? I favor trichotillomania
What is the prognosis for spontaneous recovery?
My plan is to see her if and when the dermatitis is more acute and obtain a culture to see if she has a bacterial blepharitis.


Question:
Is this eyelash trichotillomania or isolated alopecia areata of the eyelashes? I favor trichotillomania
What is the prognosis for spontaneous recovery?
My plan is to see her if and when the dermatitis is more acute and obtain a culture to see if she has a bacterial blepharitis.


Saturday, June 24, 2006
Bed Bugs
This 35 year-old man went to Mamaronek, New York to watch the New York Open Golf Championship last weekend. The closest motel room he could find was in Bridgeport, Connecticut. The latter is a city with a fairly poor reputation. Two days after returning home to Massachusetts he developed the lesions pictured here on arms and to a lesser extend on torso and legs.
They are consistent with bedbug bites (Cimex lenticularis). For a brief description go to: http://www.emedicine.com/derm/topic600.htm
In November of 2005 a bedbug epidemic was reported in New York in the New York Times. I saw a couple of cases from there here in Williamstown, MA, 150 miles away. I suppose there's a similar problem in Bridgeport now.


They are consistent with bedbug bites (Cimex lenticularis). For a brief description go to: http://www.emedicine.com/derm/topic600.htm
In November of 2005 a bedbug epidemic was reported in New York in the New York Times. I saw a couple of cases from there here in Williamstown, MA, 150 miles away. I suppose there's a similar problem in Bridgeport now.


Wednesday, June 21, 2006
Lyme Disease
This 52 year-old woman presented as a walk-in patient today. She has a five day history of an erythematous nodule on the right shoulder which has developed a ring around it. The ring measures 9 by 11 centimeters in diameter. Initially, the nodule was painful for a few days; but the pain has subsided. She has had no fever or constutional symptoms and has continued to work as a school teacher.
The patient lives in rural New Hampshire and gardens a fair bit. She was seen two times at a primary care clinic where a diagnosis of spider bite was made. First she was given Keflex, then amoxicillin.
Diagnosis: I am uncertain. I favor Lyme Disease but this has atypical features. The central nodule is unusual, although the peripheral ring looks like Lyme. I also considered atypical Sweet's Disease and a pyogenic process. Lastly, I thought of eosinophilic cellulitis (Well's Syndrome) which I have never seen.
Plan: Since she feels well, I prescribed Doxycycline 100 mg bid, and ordered a cbc, Lyme titers and a G6PD (if the lesion becomes necrotic may want to try Dapsone. I considered biopsy but was strapped for time and thought Lyme most likely. Now, I am uncertain. Biopsy will be done when she is seen in follow-up unless she is significantly better.
Your thoughts will be welcome.


Addendum:
Path Report:
DIAGNOSIS: Skin - (A) Right Shoulder-Periphery-Ring Surrounding Nodule:
Tight, mild superficial and deep perivascular lymphocytic infiltrate .
NOTE : These changes are those of a dermal hypersensitivity reaction to an exogenous antigen and, given the clinical presentation, are consistent with erythema chronicum migrans .
DIAGNOSIS: Skin - (B) Right Shoulder-Nodule:
Broad scale crust containing neutrophils , epidermal hyperplasia , marked papillary dermal edema and a superficial and deep perivascular and interstitial mixed inflammatory cell infiltrate composed of lymphocytes , neutrophils , histiocytes and plasma cells with rare eosinophils consistent with arthropod bite reactio n.
NOTE : These changes may be seen in a tick bite and erythema chronicum migrans . Clinico-pathologic correlation is suggested.
The Lyme Titer is positive.
In my opinion, this is not definitive, but the onus is on me at this time to continue to treat for Lyme.
The patient is on doxycycline and will continue on this at a dose of 100 mg bid for three weeks.
The patient reports that after three days of doxycycline the lesion is smaller. This, too, is not definitive, however, one can not ignore that either.
One Week Follow-up.
The patient feels better. Has mild insomnia.
Although initial lab titer was positive -- the Western Blot was negative indicating an early infection. Our infectious disease consultant expected them to be negative. Early treatment can prevent conversion. Will probably repeat in 2 weeks.
Picture on June 29, 2006

The patient lives in rural New Hampshire and gardens a fair bit. She was seen two times at a primary care clinic where a diagnosis of spider bite was made. First she was given Keflex, then amoxicillin.
Diagnosis: I am uncertain. I favor Lyme Disease but this has atypical features. The central nodule is unusual, although the peripheral ring looks like Lyme. I also considered atypical Sweet's Disease and a pyogenic process. Lastly, I thought of eosinophilic cellulitis (Well's Syndrome) which I have never seen.
Plan: Since she feels well, I prescribed Doxycycline 100 mg bid, and ordered a cbc, Lyme titers and a G6PD (if the lesion becomes necrotic may want to try Dapsone. I considered biopsy but was strapped for time and thought Lyme most likely. Now, I am uncertain. Biopsy will be done when she is seen in follow-up unless she is significantly better.
Your thoughts will be welcome.


Addendum:
Path Report:
DIAGNOSIS: Skin - (A) Right Shoulder-Periphery-Ring Surrounding Nodule:
Tight, mild superficial and deep perivascular lymphocytic infiltrate .
NOTE : These changes are those of a dermal hypersensitivity reaction to an exogenous antigen and, given the clinical presentation, are consistent with erythema chronicum migrans .
DIAGNOSIS: Skin - (B) Right Shoulder-Nodule:
Broad scale crust containing neutrophils , epidermal hyperplasia , marked papillary dermal edema and a superficial and deep perivascular and interstitial mixed inflammatory cell infiltrate composed of lymphocytes , neutrophils , histiocytes and plasma cells with rare eosinophils consistent with arthropod bite reactio n.
NOTE : These changes may be seen in a tick bite and erythema chronicum migrans . Clinico-pathologic correlation is suggested.
The Lyme Titer is positive.
In my opinion, this is not definitive, but the onus is on me at this time to continue to treat for Lyme.
The patient is on doxycycline and will continue on this at a dose of 100 mg bid for three weeks.
The patient reports that after three days of doxycycline the lesion is smaller. This, too, is not definitive, however, one can not ignore that either.
One Week Follow-up.
The patient feels better. Has mild insomnia.
Although initial lab titer was positive -- the Western Blot was negative indicating an early infection. Our infectious disease consultant expected them to be negative. Early treatment can prevent conversion. Will probably repeat in 2 weeks.
Picture on June 29, 2006

Wednesday, June 07, 2006
Erosio interdigitalis blastomycetica

Why do dermatologists love these cumbersome terms??
The patient is a 30 yo woman with a two week history of a sore area between the 3rd and 4th toes of the left foot. She is in good general health. Not pregnant and on no oral contraceptives. Both parents have Type II diabetes. At the time of onset she was on doxycycline for rosacea.
The examination shows an erosion in the toe web. The KOH prep was positive for pseudohyphae consistent with the diagnosis of erosio interdigitalis blastomycetica
Given her family history she should be worked up for diabetes. The doxycycline may have also played a role.
The role of maceration was discussed. She will keep toes separated and use ketoconazole cream. If this in not effective, I will ask her to dry area after bathing with a hair dryer and continue an imidazole cream or solution.
This is from emedicine.com:
Intertrigo: Intertrigo typically presents with erythema, cracking, and maceration with soreness and pruritic symptoms. Lesions typically have an irregular margin with surrounding satellite papules and pustules. Web spaces of affected fingers or toes are macerated and have the appearance of soft white skin, which is a condition termed erosio interdigitalis blastomycetica (interdigital candidosis).
A good source for the treatment of intertrigo is at: http://www.emedicine.com/derm/topic198.htm
Wednesday, May 24, 2006
Genital Pain in a 60 yo Man
Dear Pre-VGRD,
Thank you for allowing me to present this difficult case.
The patient is a 60-year-old journalist, who presents for evaluation of genital pain that has been present for about six months. He has been in his usual state of health. No new sports or traumas. His medications include atorvastin, buproprion and the generic omeprazole.
He has an annoying, painful sensation on the ventral shaft of the penis. He has noted some hyperpigmentation there and occasionally the skin here gets red. He thinks this lasts for a few hours but he is not sure. The sensation is like that of an abrasion. He saw a urologist who prescribed clobetasol cream but did not note anything in the area. He used the clobetasol for a few weeks but found that it only seemed to make the pain worse.
EXAMINATION: The examination shows a healthy, appearing 60-year-old man who is a good historian. He has a dark line on the ventral surface of the shaft of the penis. The skin here is completely normal. There was no evidence of erythema today.
IMPRESSION: This is a genital pain syndrome. It may be related to what is called scrotodynia. I also seem to remember some cases that were reported in which there was dermographic urticaria on the genitalia. I could not find references to those. The best that I can come up with at this point is a local genital pain syndrome similar to scrotodynia or vulvodynia. These are poorly understood and the treatments are not particularly effective. If this were genital dermographic urticaria, probably an antihistamine such as hydroxyzine would work.
Those of us who are dermatologists see such cases occasionally. I would appreciate your thoughts.
Marius Grenoble, QUÉBEC CITY, QC, Canada
Thank you for allowing me to present this difficult case.
The patient is a 60-year-old journalist, who presents for evaluation of genital pain that has been present for about six months. He has been in his usual state of health. No new sports or traumas. His medications include atorvastin, buproprion and the generic omeprazole.
He has an annoying, painful sensation on the ventral shaft of the penis. He has noted some hyperpigmentation there and occasionally the skin here gets red. He thinks this lasts for a few hours but he is not sure. The sensation is like that of an abrasion. He saw a urologist who prescribed clobetasol cream but did not note anything in the area. He used the clobetasol for a few weeks but found that it only seemed to make the pain worse.
EXAMINATION: The examination shows a healthy, appearing 60-year-old man who is a good historian. He has a dark line on the ventral surface of the shaft of the penis. The skin here is completely normal. There was no evidence of erythema today.
IMPRESSION: This is a genital pain syndrome. It may be related to what is called scrotodynia. I also seem to remember some cases that were reported in which there was dermographic urticaria on the genitalia. I could not find references to those. The best that I can come up with at this point is a local genital pain syndrome similar to scrotodynia or vulvodynia. These are poorly understood and the treatments are not particularly effective. If this were genital dermographic urticaria, probably an antihistamine such as hydroxyzine would work.
Those of us who are dermatologists see such cases occasionally. I would appreciate your thoughts.
Marius Grenoble, QUÉBEC CITY, QC, Canada
Thursday, May 18, 2006
Photosensitive dermatitis from bleaching creams




My friend, David Elpern MD, a dermatologist from Williamstown, USA sent this note to me.
"NY Times
May 14, 2006
A Vision of Pale Beauty Carries Risks for Asia's Women
By THOMAS FULLER
MAKHAM KHU, Thailand - Neighbors gawk and children yell, "Ghost!" The manager of the restaurant where Panya Boonchun worked simply told her she was fired.
The cream that she applied to her face and neck was supposed to transform her into a white-skinned beauty, the kind she saw in women's magazines and on television.
But the illegally produced lotion she bought in a store near this village in southeastern Thailand turned her skin into a patchwork of albino pink and dark brown. Doctors say her condition may be irreversible.
"I never look in the mirror anymore," she said, sobbing during an interview.
Whiter skin is being aggressively marketed across Asia, with vast selections of skin-whitening creams on supermarket and pharmacy shelves testament to an industry that has flourished over the past decade. In Hong Kong, Malaysia, the Philippines, South Korea and Taiwan, 4 of every 10 women use a whitening cream, a survey by Synovate, a market research company, found."
And it so happened the same morning I saw a 33-year-old man who had been applying a bleaching cream from Southern Thailand for his melasma. After several weeks of application, He noticed pigmentary changes on his face which was dusky brownish tinge on the forehead, cheeks and chin. It has now spread to the neck as well. Past one week, he noticed skin eruptions appearing on the forearms as well. He was otherwise well and has no fever or polyarthralgia.
His medication history included OTC garlic pills and fish oil. He is however a heavy drinker.
Examination of the skin showed diffuse dusky erythematous to brownish macules on the patient's ears, face and neck. The eruptions somehow spares the nose. Eczematous eruptions were noted on the forearms bilaterally. There were no hepatosplenomegaly. There were no sclerodactyly changes on the fingers.
My first impression was could this be the "southern thailand bleaching creams ghostly onchronosis due to high concentration hydroquinone cream??
Investigations done showed normal blood counts and blood biochemistry. ANA serology was negative.
I suspect this is some form of photosensitive dermatitis. Porphyria cutanea tarda runs thro my mind as a differential as he is heavy drinker but his LFTs were normal. I have never seen this before.
Wednesday, May 17, 2006
Onycholysis
The patient is a healthy 58 year old woman with a 3 year history of onycholysis. Fungal culture has grown out Candida zeylanoides. Bacterial culture negative.
Topicals have not been of help. (imidazoles and thymol in chloroform)
Would fluconazole be of value?
Should the nail be avulsed?
Who has had success treating this kind of problem?

Topicals have not been of help. (imidazoles and thymol in chloroform)
Would fluconazole be of value?
Should the nail be avulsed?
Who has had success treating this kind of problem?

Thursday, May 11, 2006
Pellagra in Alcoholics
In Iraq, pellagra is only seen in sporadic cases in patients with alcoholism. I describe here a case of pellagra in 30 year old man who used to drink alcohol one litre a day of a local beverage called ARAK. In addition, his nutrition was poor. He developed a typical rash of pellagra in photosensitive area, some lesions are bullous together with beefy tongue. The rash resolved quickly after vitamin replacement but recurred when he resumed alcohol drinking.
I would like to ask my colleagues
1) how often see pellagra
2) what is the cause?





I would like to ask my colleagues
1) how often see pellagra
2) what is the cause?





Tuesday, May 09, 2006
Nail Bed Carcinoma
The patient is s 70 yo man who was seen today for a three year follow-up of micrographic surgery for a sqaumous cell carcinoma of the nail bed. There is no evidence of recurrence and the results are cosmetically excellent.
I had another patient with a similar lesion. He was a VA patient and they did not approve him for microgrpahic surgery. He had the distal part of his thumb excised. Bizarre that health insurance trumps the interests of the patient.

I had another patient with a similar lesion. He was a VA patient and they did not approve him for microgrpahic surgery. He had the distal part of his thumb excised. Bizarre that health insurance trumps the interests of the patient.
