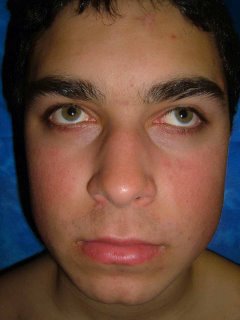
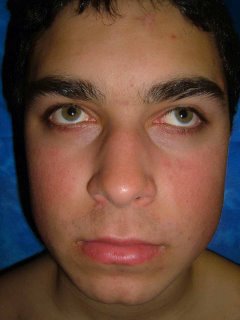
The patient is a 15 year old boy with a many year history of ruddy cheeks and a fine follicular eruption in the affected areas. He also has typical keratosis pilaris on his arms and thighs. The diagnosis of erythromelanosis follicularis of the face (also called keratosis pilaris rubra facei) is not difficult. Who has a therapeutic suggestion? I don't think the patient is ready for laser therapy yet. It was difficult to capture the depth of the erythema here which is qute striking. His sister has a similar process but is is milder.


Reference:
Stephan F, Ayoub N, Klein-Tomb L, Tomb R.
[Erythromelanosis follicularis faciei and colli]
Ann Dermatol Venereol. 2002 Jan;129(1 Pt 1):63-5. [Article in French]
BACKGROUND: Erythromelanosis follicularis of the face and neck, originally
described in Japan by Kitamura et al. in 1960, is characterized by a clinical
set of three: well-demarcated erythema, hyperpigmentation and follicular
papules. It affects the face and the neck generally on both sides. Since the
original description, it has seldom been reported in the literature. CASE
REPORTS: This paper reports two patients with unilateral presentation.
DISCUSSION: Having discussed the various differential diagnoses all published
cases were listed and analyzed. The prevalence of this disease appears higher
than is shown by the limited number of cases reported in the literature. It
deserves more recognition. Its nosologic and aetiologic frames still remain to
be clarified.


 55 year old man with 6 month history of nail distrophy. Only thumbs. He works with his hands cutting film. Trauma likely.
55 year old man with 6 month history of nail distrophy. Only thumbs. He works with his hands cutting film. Trauma likely.